Volume 11, Issue 1 (7-2023)
Jorjani Biomed J 2023, 11(1): 13-15 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Fahim Yeganeh S A, Raghimi H, Mohammadi M R. Epidemiologic and clinical manifestation analysis of COVID-19 patients admitted to 5th Azar Hospital in Gorgan. Jorjani Biomed J 2023; 11 (1) :13-15
URL: http://goums.ac.ir/jorjanijournal/article-1-943-en.html
URL: http://goums.ac.ir/jorjanijournal/article-1-943-en.html
1- Department of Emergency Medicine, School of Medicine, 5 Azar Hospital, Golestan University of Medical Sciences, Gorgan, IRAN
2- Clinical Research Development Unit (CRDU), 5 Azar Hospital, Golestan University of Medical Sciences, Gorgan, Iran
3- Department of Neurosurgery, School of Medicine, 5 Azar Hospital, Golestan University of Medical Sciences, Gorgan, IRAN ,mr_mohammadi_md@yahoo.com
2- Clinical Research Development Unit (CRDU), 5 Azar Hospital, Golestan University of Medical Sciences, Gorgan, Iran
3- Department of Neurosurgery, School of Medicine, 5 Azar Hospital, Golestan University of Medical Sciences, Gorgan, IRAN ,
Full-Text [PDF 426 kb]
(1297 Downloads)
| Abstract (HTML) (3993 Views)
Full-Text: (815 Views)
Introduction
Contagious, deadly new viral infection (COVID-19), a beta coronavirus closely similar to the SARS virus, was first seen in Wuhan, China, in December 2019 (1). An illness that invades the targets via inhaling droplets of the contaminated victims. Clinical symptoms include simple cold-like syndrome, a severe intractable fever, cough, hypoxia, and pneumonia with or without ARDS, leading to death in severely involved people.
After involvement, a series of events occur, such as activation of cytokines and chemokines with infiltration of inflammatory cells and apoptosis in the epithelial layer of the airway mucosa. Hypoxia, sepsis, and multi-organ failure are severe, leading to death (2).
Considering the global priority of the disease, it is vital to identify the epidemiological and clinical patterns of this disease and estimate its characteristics concerning the severity of the disease in order to control it (3). Studies have shown that at least one-third of cases of COVID-19 infection are asymptomatic. In addition, almost three-quarters of people who were asymptomatic at the time of PCR testing remained asymptomatic at follow-up (4).
The most reported symptoms in COVID-19 patients are fever or chills, headache, muscle or body pain, dry cough, fatigue, shortness of breath, decreased leukocytes, and radiographic evidence of pneumonia. Less reported symptoms include diarrhea, runny nose, liver and kidney damage, nausea, vomiting, lymphopenia, and thrombocytopenia. Symptoms begin 2 to 14 days after exposure to the virus (5-8).
High-resolution spiral CT scan of lungs with 98% sensitivity helps physicians to start treatment as soon as possible (9,10). RT-PCR test takes time to respond, so the patients were admitted with suspicious signs and symptoms with positive CT scan findings. The PCR test was sent for all of them. Some factors, such as the age of the patient, gender, co-morbidities, clinical condition of the patient, and drug use, are the most important predictors of clinical results and disease severity in patients (11).
5th Azar Hospital admits only adult people more than 18 years old. The treatment was based on protocols the WHO and the Ministry of Health and Treatment of Iran advised. Considering the profound impact of COVID-19 on the community, this study aimed to evaluate and report the clinical condition of patients and the symptoms involved, which can greatly help disease management in regional and national analyses. Thus, the present study aimed to survey epidemiologic and clinical manifestations of COVID-19 patients admitted to the hospital.
Methods
This cross-sectional study was done in May and June 2020 with 200 cases. Positive signs and symptoms plus active CT scan findings were the first steps of diagnosis and admission. The PCR test was sent for all of them. 5th Azar Hospital admits only adult people more than 18 years old. This hospital is a referral in Golestan province for COVID-19.
Demographic information and laboratory tests were extracted by history, medical documents, and follow-up by phone later. All data was recorded about their age, gender, underlying disease, accompanying symptoms, and involvement of other close family members. They were asked to participate in every kind of gathering and ceremony. Patients were followed for at least six months.
All cases in this study underwent a spiral CT scan of the chest and RT-PCR test. Other essential work-ups were also done to obtain more information about the patient’s condition. The authors got all data history-wise, hospital medical documents, and follow-up done by phone contact. A radiologist reported all CT scans, and an emergency medicine physician reviewed them. All these patients were admitted to the hospital. A Spiral CT scan of the lungs was done and reported by a radiologist. Due to the severity of the involvement of parenchyma, the authors categorized them as mild (< 20%), moderate (20 – 50%), and severe (>50%). The abnormality of CT scan findings were ground glass opacity, pleural effusion, and consolidation (R). This study started after the agreement of the Deputy of Research of Golestan University of Medical Sciences and getting an ethical code from the Medical Ethics Committee (IR.GOUMS.REC.1399.421). Statistical evaluation was done with SPSS-16 using the chi-square test and descriptive analysis.
Results
This study had 200 cases with signs and symptoms of COVID-19. They were referred to the emergency room outpatient clinic, 5th Azar Hospital in Gorgan (north of Iran), and visited in May and June 2020. The mean age was (57.25 ± 16.8), and the age range was between 19 and 93. 5th Azar Hospital accepts adult patients. One hundred fifty-three patients (76.5%) had positive RT-PCR for COVID-19. The most common complaints were shortness of breath (n=139, 69.5%), fever (n=102, 51%), cough (n=100, 50%), weakness, and lethargy (n=92, 46%). See more information in Table 1.
Positive RT-PCR was obtained from 153 patients (76.5%). Of fifty-eight patients with severe involvement of the lungs, forty-seven (81%) had positive PCR. In other patients, this record was 106 (74.6%).
In this study, sixty-seven patients (33.5%) simultaneously had at least one close family member infected with COVID-19. Seven out of fifty-eight (12.1%) patients with severe involvement of lungs (>50%) expired, but in the mild and moderate groups, there was ten out of 142 (7%) mortality.
106 out of 142 cases (74.6%) had positive PCR tests in the mild and moderate groups. In patients with severe involvement, forty-seven out of fifty-eight patients (81%) had positive PCR tests.
One hundred thirteen (56.5%) cases had a history of recent participation in groups and gatherings.
Diabetes mellitus (DM) (n=70, 35%), hypertension (n=47, 23.5%), and cardiovascular disease (CVD) (n=19, 9.5%) were reported as major underlying diseases seen in patients. There were eighty-one (40.5%) patients without any underlying disease. Ninety-one (45.5%) had only one type, twenty (10%) had two types, seven (3.5%) had three types, and one (0.5%) had four types of underlying disease (DM, HTN, heart disease, or immune deficiency) before admission.
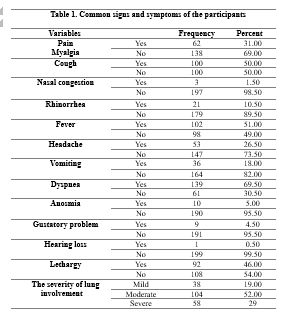
A Spiral CT scan of the chest showed thirty-eight (19%) cases with mild (< 20%), 104 (52%) moderate (20 – 50%), and fifty-eight (29%) cases with severe (> 50%) involvement of lung parenchyma (Table 1). There was no significant difference between males and females (P> 0.05). In this study, 125 (62.5%) live in urban areas and seventy-five (37.5%) in rural areas. There were seventy (35%) patients with a history of DM. Among these seventy diabetic patients, six cases were in the expired patient group. Additionally, six out of 19 patients in the heart disease group died. Forty-seven (23.5%) patients had hypertension, and 19 (9.5%) had heart disease. There were eight expired patients among forty-seven cases of hypertension.
Correlation of CT findings with DM showed diabetic patients (n=44, 62.9%) had mild and moderate lung involvement. Severe involvement was seen in twenty-six (37.1%) cases.
Of deceased patients, three (17.6%) had no underlying disease. The remaining (n=14, 82.4%) had at least one type of disease. Seventeen (8.5%) patients expired due to COVID-19 involvement and complications. The mean age of patients who survived was 56.37±16.36, and the expired patients reported 66.70±19.77. All deceased patients expired during admission to the hospital. Although the severity of CT scan findings within the expired patients was more than survived, the relation was insignificant (P=0.247).
DM had significant relation with the severity of CT scan findings (P=0.029). Hypertension had no significant relation to the severity of CT scan findings (P=0.487). Patients with at least one type of underlying disease had a significant association (P=0.045) with patients who died. Hypertension was more in expired patients and had a significant relation (P=0.023).
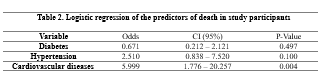
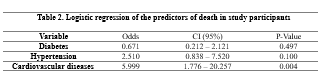
CVD patients had a mortality risk of 5.9 folds compared to patients free of CVD (Table 2).
Discussion
This study reported 200 cases with clinical manifestations of COVID-19 accompanied by positive CT scan findings. All were admitted to the hospital for better evaluation of disease severity. RT-PCR has been done entirely.
In this report, the mean age was 57 years old. Similar results were seen in Wong et al. (mean=56 years old) (12), Chen et al. (13), and Shahriarirad et al. (mean=53.75 years old) studies (14). There were insignificant differences in these series. The age range was 19-93 years old. In addition , other studies confirm such findings (12,13,15).
This study had 153 (76.5%) positive RT-PCR tests. Due to the possibility of false-negative reports of PCR, medical treatment is initiated with diagnosis based on signs and symptoms with positive related CT scan findings (16).
Maximum complaints were dyspnea (shortness of breath) (n=139, 69.5%), fever (n=102, 51%), cough (n=100, 50%), weakness, and lethargy (n=92, 46%). Similar findings could be seen in other studies, confirming that fever and cough are the most common symptoms (14, 16, 17). Wong et al. reported a fever in 80% and a cough in 50% of patients (10). Adhikari et al. reported the same results (18). Guan et al. found a fever in 87.9% and a cough in 67.7% of cases (19). Wong et al. reported high fever in 22% and mild fever in 38% of patients (12).
Dyspnea (shortness of breath) was the most common symptom (69.5% of patients). Chen et al. reported dyspnea in 31% and Shahriarirad et al. in 58% of their patients in Shiraz. Headache (26.5%) and vomiting (18%) were not common findings as previous results. In many other reports, they were rare findings. Chen et al. reported headache at 8% and vomiting at 1% (13). Shahriarirad et al. found headache at 53.1% and vomiting at 25.7% (14).
Rhinorrhea (10.5%) and altered smelling sense (5%) were reported in this study. In Shahriarirad et al. study, rhinorrhea was 23% (14). Taziki et al. reported olfactory and gustatory dysfunction as a complaint of people involved with COVID-19. They reported a complete recovery in six months is 98.8% (20).
Underlying diseases, a debilitating factor in people infected with COVID-19, make a major challenge for physicians responsible for treating patients. The recent study had patients with DM (n=70, 35%), hypertension (n=47, 23.5%), and CVD (n=9, 9.5%). There were ninety-one patients (45.5%) with only one type of mentioned diseases, twenty (10%) with two types, and seven (3.5%) with three types of underlying problems. Wong et al. reported hypertension (20%) and diabetes (13%) (12). Besides, Shahriarirad et al. reported hypertension 19.5% and diabetes 14.2% (14). Additionally, Hwang et al. reported hypertension (15%), diabetes (20%), and CVD (15%) (21). Lake also reported diabetes at 20%, hypertension at 15%, and CVD at 15% (22).
Seventeen (8.5%) patients expired during admission to the hospital. Li et al. reported 5% mortality (23). Huang et al. showed 15% fatality (21). Shahriarirad et al. had 8% mortality (14). Chen et al. reported an 11% mortality rate (13). Chan et al. reported family clusters in their series. In this study, 33.5% of at least one close family member was involved simultaneously (13).
Conclusion
After the outbreak of COVID-19 in China and the spread of this infection to many countries, there were waves of infected patients referred to the 5th Azar Hospital. Based on this study (200 cases), age and underlying diseases were the main predicting factors for prognosis.
Acknowledgment
The authors thank Miss Sepideh Sadat Hosseini for her kindly cooperation.
Ethical statement
This study derived from the thesis of Haniyeh Ragimi (Intern in medical school) at Golestan University of Medical Sciences and the agreement of the Deputy of Research (GOUMS) and getting Ethical Code (IR.GOUMS.REC.1399.421). All cases signed informed consent and responded to phone calls ambitiously. All data will remain confidential.
Conflict of interest
The authors declared no conflict of interest.
Contagious, deadly new viral infection (COVID-19), a beta coronavirus closely similar to the SARS virus, was first seen in Wuhan, China, in December 2019 (1). An illness that invades the targets via inhaling droplets of the contaminated victims. Clinical symptoms include simple cold-like syndrome, a severe intractable fever, cough, hypoxia, and pneumonia with or without ARDS, leading to death in severely involved people.
After involvement, a series of events occur, such as activation of cytokines and chemokines with infiltration of inflammatory cells and apoptosis in the epithelial layer of the airway mucosa. Hypoxia, sepsis, and multi-organ failure are severe, leading to death (2).
Considering the global priority of the disease, it is vital to identify the epidemiological and clinical patterns of this disease and estimate its characteristics concerning the severity of the disease in order to control it (3). Studies have shown that at least one-third of cases of COVID-19 infection are asymptomatic. In addition, almost three-quarters of people who were asymptomatic at the time of PCR testing remained asymptomatic at follow-up (4).
The most reported symptoms in COVID-19 patients are fever or chills, headache, muscle or body pain, dry cough, fatigue, shortness of breath, decreased leukocytes, and radiographic evidence of pneumonia. Less reported symptoms include diarrhea, runny nose, liver and kidney damage, nausea, vomiting, lymphopenia, and thrombocytopenia. Symptoms begin 2 to 14 days after exposure to the virus (5-8).
High-resolution spiral CT scan of lungs with 98% sensitivity helps physicians to start treatment as soon as possible (9,10). RT-PCR test takes time to respond, so the patients were admitted with suspicious signs and symptoms with positive CT scan findings. The PCR test was sent for all of them. Some factors, such as the age of the patient, gender, co-morbidities, clinical condition of the patient, and drug use, are the most important predictors of clinical results and disease severity in patients (11).
5th Azar Hospital admits only adult people more than 18 years old. The treatment was based on protocols the WHO and the Ministry of Health and Treatment of Iran advised. Considering the profound impact of COVID-19 on the community, this study aimed to evaluate and report the clinical condition of patients and the symptoms involved, which can greatly help disease management in regional and national analyses. Thus, the present study aimed to survey epidemiologic and clinical manifestations of COVID-19 patients admitted to the hospital.
Methods
This cross-sectional study was done in May and June 2020 with 200 cases. Positive signs and symptoms plus active CT scan findings were the first steps of diagnosis and admission. The PCR test was sent for all of them. 5th Azar Hospital admits only adult people more than 18 years old. This hospital is a referral in Golestan province for COVID-19.
Demographic information and laboratory tests were extracted by history, medical documents, and follow-up by phone later. All data was recorded about their age, gender, underlying disease, accompanying symptoms, and involvement of other close family members. They were asked to participate in every kind of gathering and ceremony. Patients were followed for at least six months.
All cases in this study underwent a spiral CT scan of the chest and RT-PCR test. Other essential work-ups were also done to obtain more information about the patient’s condition. The authors got all data history-wise, hospital medical documents, and follow-up done by phone contact. A radiologist reported all CT scans, and an emergency medicine physician reviewed them. All these patients were admitted to the hospital. A Spiral CT scan of the lungs was done and reported by a radiologist. Due to the severity of the involvement of parenchyma, the authors categorized them as mild (< 20%), moderate (20 – 50%), and severe (>50%). The abnormality of CT scan findings were ground glass opacity, pleural effusion, and consolidation (R). This study started after the agreement of the Deputy of Research of Golestan University of Medical Sciences and getting an ethical code from the Medical Ethics Committee (IR.GOUMS.REC.1399.421). Statistical evaluation was done with SPSS-16 using the chi-square test and descriptive analysis.
Results
This study had 200 cases with signs and symptoms of COVID-19. They were referred to the emergency room outpatient clinic, 5th Azar Hospital in Gorgan (north of Iran), and visited in May and June 2020. The mean age was (57.25 ± 16.8), and the age range was between 19 and 93. 5th Azar Hospital accepts adult patients. One hundred fifty-three patients (76.5%) had positive RT-PCR for COVID-19. The most common complaints were shortness of breath (n=139, 69.5%), fever (n=102, 51%), cough (n=100, 50%), weakness, and lethargy (n=92, 46%). See more information in Table 1.
Positive RT-PCR was obtained from 153 patients (76.5%). Of fifty-eight patients with severe involvement of the lungs, forty-seven (81%) had positive PCR. In other patients, this record was 106 (74.6%).
In this study, sixty-seven patients (33.5%) simultaneously had at least one close family member infected with COVID-19. Seven out of fifty-eight (12.1%) patients with severe involvement of lungs (>50%) expired, but in the mild and moderate groups, there was ten out of 142 (7%) mortality.
106 out of 142 cases (74.6%) had positive PCR tests in the mild and moderate groups. In patients with severe involvement, forty-seven out of fifty-eight patients (81%) had positive PCR tests.
One hundred thirteen (56.5%) cases had a history of recent participation in groups and gatherings.
Diabetes mellitus (DM) (n=70, 35%), hypertension (n=47, 23.5%), and cardiovascular disease (CVD) (n=19, 9.5%) were reported as major underlying diseases seen in patients. There were eighty-one (40.5%) patients without any underlying disease. Ninety-one (45.5%) had only one type, twenty (10%) had two types, seven (3.5%) had three types, and one (0.5%) had four types of underlying disease (DM, HTN, heart disease, or immune deficiency) before admission.
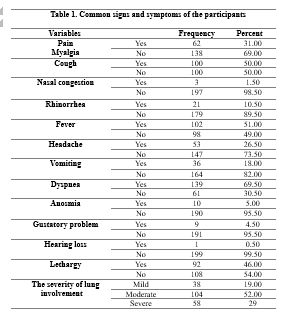
A Spiral CT scan of the chest showed thirty-eight (19%) cases with mild (< 20%), 104 (52%) moderate (20 – 50%), and fifty-eight (29%) cases with severe (> 50%) involvement of lung parenchyma (Table 1). There was no significant difference between males and females (P> 0.05). In this study, 125 (62.5%) live in urban areas and seventy-five (37.5%) in rural areas. There were seventy (35%) patients with a history of DM. Among these seventy diabetic patients, six cases were in the expired patient group. Additionally, six out of 19 patients in the heart disease group died. Forty-seven (23.5%) patients had hypertension, and 19 (9.5%) had heart disease. There were eight expired patients among forty-seven cases of hypertension.
Correlation of CT findings with DM showed diabetic patients (n=44, 62.9%) had mild and moderate lung involvement. Severe involvement was seen in twenty-six (37.1%) cases.
Of deceased patients, three (17.6%) had no underlying disease. The remaining (n=14, 82.4%) had at least one type of disease. Seventeen (8.5%) patients expired due to COVID-19 involvement and complications. The mean age of patients who survived was 56.37±16.36, and the expired patients reported 66.70±19.77. All deceased patients expired during admission to the hospital. Although the severity of CT scan findings within the expired patients was more than survived, the relation was insignificant (P=0.247).
DM had significant relation with the severity of CT scan findings (P=0.029). Hypertension had no significant relation to the severity of CT scan findings (P=0.487). Patients with at least one type of underlying disease had a significant association (P=0.045) with patients who died. Hypertension was more in expired patients and had a significant relation (P=0.023).
CVD patients had a mortality risk of 5.9 folds compared to patients free of CVD (Table 2).
Discussion
This study reported 200 cases with clinical manifestations of COVID-19 accompanied by positive CT scan findings. All were admitted to the hospital for better evaluation of disease severity. RT-PCR has been done entirely.
In this report, the mean age was 57 years old. Similar results were seen in Wong et al. (mean=56 years old) (12), Chen et al. (13), and Shahriarirad et al. (mean=53.75 years old) studies (14). There were insignificant differences in these series. The age range was 19-93 years old. In addition , other studies confirm such findings (12,13,15).
This study had 153 (76.5%) positive RT-PCR tests. Due to the possibility of false-negative reports of PCR, medical treatment is initiated with diagnosis based on signs and symptoms with positive related CT scan findings (16).
Maximum complaints were dyspnea (shortness of breath) (n=139, 69.5%), fever (n=102, 51%), cough (n=100, 50%), weakness, and lethargy (n=92, 46%). Similar findings could be seen in other studies, confirming that fever and cough are the most common symptoms (14, 16, 17). Wong et al. reported a fever in 80% and a cough in 50% of patients (10). Adhikari et al. reported the same results (18). Guan et al. found a fever in 87.9% and a cough in 67.7% of cases (19). Wong et al. reported high fever in 22% and mild fever in 38% of patients (12).
Dyspnea (shortness of breath) was the most common symptom (69.5% of patients). Chen et al. reported dyspnea in 31% and Shahriarirad et al. in 58% of their patients in Shiraz. Headache (26.5%) and vomiting (18%) were not common findings as previous results. In many other reports, they were rare findings. Chen et al. reported headache at 8% and vomiting at 1% (13). Shahriarirad et al. found headache at 53.1% and vomiting at 25.7% (14).
Rhinorrhea (10.5%) and altered smelling sense (5%) were reported in this study. In Shahriarirad et al. study, rhinorrhea was 23% (14). Taziki et al. reported olfactory and gustatory dysfunction as a complaint of people involved with COVID-19. They reported a complete recovery in six months is 98.8% (20).
Underlying diseases, a debilitating factor in people infected with COVID-19, make a major challenge for physicians responsible for treating patients. The recent study had patients with DM (n=70, 35%), hypertension (n=47, 23.5%), and CVD (n=9, 9.5%). There were ninety-one patients (45.5%) with only one type of mentioned diseases, twenty (10%) with two types, and seven (3.5%) with three types of underlying problems. Wong et al. reported hypertension (20%) and diabetes (13%) (12). Besides, Shahriarirad et al. reported hypertension 19.5% and diabetes 14.2% (14). Additionally, Hwang et al. reported hypertension (15%), diabetes (20%), and CVD (15%) (21). Lake also reported diabetes at 20%, hypertension at 15%, and CVD at 15% (22).
Seventeen (8.5%) patients expired during admission to the hospital. Li et al. reported 5% mortality (23). Huang et al. showed 15% fatality (21). Shahriarirad et al. had 8% mortality (14). Chen et al. reported an 11% mortality rate (13). Chan et al. reported family clusters in their series. In this study, 33.5% of at least one close family member was involved simultaneously (13).
Conclusion
After the outbreak of COVID-19 in China and the spread of this infection to many countries, there were waves of infected patients referred to the 5th Azar Hospital. Based on this study (200 cases), age and underlying diseases were the main predicting factors for prognosis.
Acknowledgment
The authors thank Miss Sepideh Sadat Hosseini for her kindly cooperation.
Ethical statement
This study derived from the thesis of Haniyeh Ragimi (Intern in medical school) at Golestan University of Medical Sciences and the agreement of the Deputy of Research (GOUMS) and getting Ethical Code (IR.GOUMS.REC.1399.421). All cases signed informed consent and responded to phone calls ambitiously. All data will remain confidential.
Conflict of interest
The authors declared no conflict of interest.
Type of Article: Original article |
Subject:
General medicine
Received: 2022/12/15 | Accepted: 2023/02/12 | Published: 2023/07/1
Received: 2022/12/15 | Accepted: 2023/02/12 | Published: 2023/07/1
References
1. World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: Interim guidance. Ginebra; 2020. p.21 Monography in English | BIGG - GRADE guidelines. [View at Publisher] [DOI] [Google scholar]
2. Siordia Jr JA. Epidemiology and clinical features of COVID-19: A review of current literature. J Clin Virol. 2020;127:104357. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Maleki M, Mahmoudi MR, Heydari MH, Pho KH. Modeling and forecasting the spread and death rate of coronavirus (COVID -19) in the world using time series models. Chaos Solitons Fractals. 2020;140:110151. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Oran DP, Topol EJ. The Proportion of SARS-Cov-2 Infections that are Asymptomatic: A Systematic Review. Ann Intern Med. 2021; 174(5): 655-62. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (1): A Review. JAMA. 2020;324(8):782-93. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Harapan H, Itoh N, Yufika A, Winardi W, Keam S, Te H, et al. Coronavirus Disease 2019 (COVID-19): A Literature Review. J Infection and Public Health. 2020;13(5):667-73. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Wu J, Li J, Zhu G, Zhang Y, Bi Z, Yu Y, et al. Clinical Features of Maintenance Hemodialysis Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. Clin J Am Soc Nephrol. 2020;15(8):1139-45. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Li T, Wei C, Li W, Hongwei F, Shi J. Beijing :union: Medical College Hospital on "Pneumonia of Novel Coronavirus Infection" Diagnosis and Treatment Proposal (V2. 0). Med J Peking :union: Med Coll Hosp. 2020. [View at Publisher]
9. Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W. Sensitivity of Chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296(2):E115-7. [View at Publisher] [DOI] [PMID] [Google scholar]
10. Kim H, Hong H, Yoon SH. Diagnostic Performance of CT and Reverse Transcriptase Polymerase Chain Reaction for Coronavirus Disease 2019: A Meta-Analysis. Radiology. 2020;296(3):E145-55. [View at Publisher] [DOI] [PMID] [Google scholar]
11. Sabri A, Davarpanah AH, Mahdavi A, Abrishami A, Khazaei M, Heydari S, et al. Novel coronavirus disease 2019: predicting prognosis with a computed tomography -based disease severity score and clinical laboratory data. Pol Arch Intern Med. 2020;130(7-8):629-34. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Wong HYF, Lam HYS, Fong AH, Leung ST, Chin TW, Lo CSY, et.al. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology. 2020;296(2):E72-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et.al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395(10223):507-13. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Shahriarirad R, Khodamoradi Z, Erfani A, Hosseinpour H, Ranjbar K, Emami Y, et.al. Epidemiological and clinical features of 2019 novel coronavirus diseases (COVID-19) in the South of Iran. BMC Infect Dis. 2020;20(1):427. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV). Radiology. 2020;295(1):202-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Nematollahi N, Mohammadi MR, Vakili MA, Baniaghil AS, Ghelichli M, Najafi MJ, et al. Chest CT Findings (COVID-19), Analysis of 200 Cases (Postmortem). J Adv Med Biomed Res. 2022;30(140):241-8. [View at Publisher] [DOI] [Google scholar]
17. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et.al. Time Course of Lung Changes at Chest CT during Recovery from Coronavirus Disease 2019 (COVID-19). Radiology. 2020; 295(3):715-21. [View at Publisher] [DOI] [PMID] [Google scholar]
18. Adhikari SP, Meng S, Wu YJ, Mao YP, Ye RX, Wang QZ, et.al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty. 2020;9(1):29. [View at Publisher] [DOI] [PMID] [Google scholar]
19. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et.al. China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20. [View at Publisher] [DOI] [PMID] [Google scholar]
20. Taziki Balajelini MH, Vakili MA, Rajabi A, Mohammadi M, Tabarraei A, Hosseini SM. Recovery of olfactory and gustatory dysfunctions in coronavirus disease 2019 patients: a prospective cohort study. J Laryngol Otol. 2022:1-8. [View at Publisher] [DOI] [PMID] [Google scholar]
21. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et.al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Lake MA. What we know so far: COVID-19 current clinical knowledge and research. Clin Med (Lond). 2020; 20(2):124-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et.al. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 2020;92(6):577-83. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |