Volume 12, Issue 4 (12-2024)
Jorjani Biomed J 2024, 12(4): 22-25 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Alizadeh-Barzian K, Nikkhooy Z, Soltani R, Jamshidi M, Sabaghan M, Difrakhsh A, et al . Epidemiologic, demographic, and clinical characteristics of brucellosis in Behbahan County, Southwest Iran, during the years 2000-2021. Jorjani Biomed J 2024; 12 (4) :22-25
URL: http://goums.ac.ir/jorjanijournal/article-1-1047-en.html
URL: http://goums.ac.ir/jorjanijournal/article-1-1047-en.html
Kazem Alizadeh-Barzian1 

 , Zahra Nikkhooy1
, Zahra Nikkhooy1 

 , Rahmatollah Soltani2
, Rahmatollah Soltani2 

 , Mehdi Jamshidi1
, Mehdi Jamshidi1 

 , Mohamad Sabaghan1
, Mohamad Sabaghan1 

 , Abolhasan Difrakhsh1
, Abolhasan Difrakhsh1 

 , Roya Ghanavati1
, Roya Ghanavati1 

 , Masoud Parash1
, Masoud Parash1 

 , Ali Jamshidi3
, Ali Jamshidi3 




 , Zahra Nikkhooy1
, Zahra Nikkhooy1 

 , Rahmatollah Soltani2
, Rahmatollah Soltani2 

 , Mehdi Jamshidi1
, Mehdi Jamshidi1 

 , Mohamad Sabaghan1
, Mohamad Sabaghan1 

 , Abolhasan Difrakhsh1
, Abolhasan Difrakhsh1 

 , Roya Ghanavati1
, Roya Ghanavati1 

 , Masoud Parash1
, Masoud Parash1 

 , Ali Jamshidi3
, Ali Jamshidi3 


1- Behbahan Faculty of Medical Sciences, Behbahan, Iran
2- Clinical Education Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
3- Behbahan Faculty of Medical Sciences, Behbahan, Iran ,jamshidiali91@yahoo.com
2- Clinical Education Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
3- Behbahan Faculty of Medical Sciences, Behbahan, Iran ,
Full-Text [PDF 322 kb]
(320 Downloads)
| Abstract (HTML) (3406 Views)
Discussion
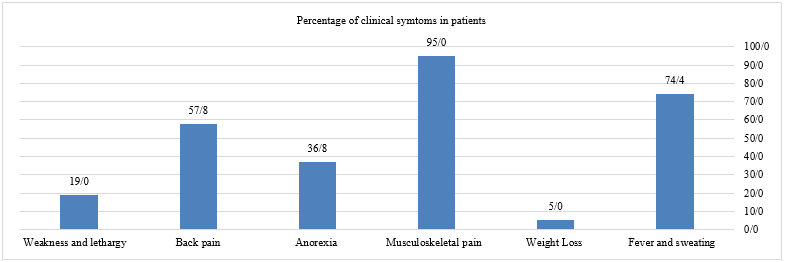
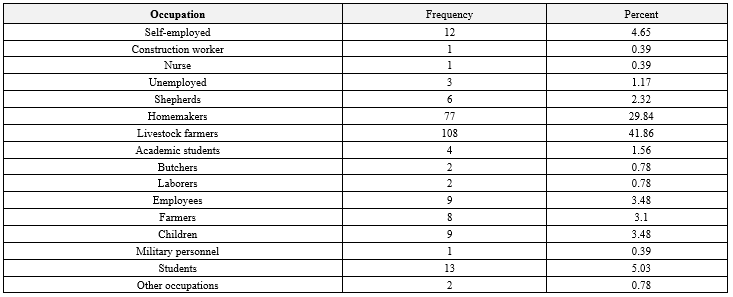
Although brucellosis has been eradicated in some countries, it still exists as an endemic health problem in our country (9). According to the WHO, the incidence of this disease ranges from 0.01 to 200 per 100,000 people, and the prevalence varies from 0.5 per 100 people to 9.10 per 100 people in different provinces of Iran (10). Based on the findings of this study, the incidence of brucellosis in Behbahan County during the period of 2000-2021 was an average of 0.6 per 100,000 individuals. A similar study conducted by Jelastopulu et al. demonstrated that through vaccination of livestock and public education in western Greece the incidence of brucellosis could be reduced from 10 per 100,000 individuals (1998-1997) to 0.3 per 1,000 individuals (2002-2000) (11). The history of patient contact with livestock and unsterilized livestock products, especially unsterilized dairy products, had the highest percentage (88.8%), while the lowest percentage (13.02%) was related to contact with animal slaughter, blood, and secretions. This may indicate that the climatic characteristics of Behbahan County contribute to a higher presence of livestock in the region, which in turn leads to more opportunities for contact with livestock. In a similar study conducted by Ghasemi et al. in Kurdistan province, the most common mode of disease transmission was contact with contaminated animals and the consumption of contaminated animal products (48.3%). Disease transmission by eating contaminated animal products alone (7.36%) or by contact with contaminated animals alone (6.10%) had a lower prevalence (12). Livestock farmers account for 42% of the patients compared to other occupations in Behbahan County, confirming the previous conclusion that the level of contact with livestock is high in the region. In a similar study conducted by Shahriari et al. in Kohgiluyeh and Boyer-Ahmad provinces in 2009-2013, it was found that 84% had a history of contact with livestock, and 31.5% were livestock farmers or slaughterhouse workers (6). In this study, men (53%) were more affected than women (47%). A study conducted by Hosseini et al. in Amol County also showed a higher incidence in males compared to females (13). Another study conducted by Hamzavi et al. in Kermanshah province showed a higher incidence in males compared to females, which is consistent with the current study (14). The higher incidence of brucellosis in men compared to women is probably attributed to the type of work and increased contact with livestock and their products. In the current study, the majority of cases were rural residents (54%). In a similar study conducted by Hosseini et al. in Amol County, the incidence of brucellosis was higher among rural residents (68.21%) compared to urban residents (31.79%) (13). In another similar study conducted by Farahani et al. in Arak County, the majority of brucellosis cases were among rural residents (72%) compared to urban residents (28%) (15). The overall incidence of brucellosis was higher in the rural population compared to the urban population. There is a significant association between gender and livestock. In rural populations, the incidence of brucellosis is higher in men than women, and contact with livestock is likely considered a primary mode of transmission for women in these areas. Since contact with livestock and handling of fetal products is more likely to be performed by men in the current living conditions of rural communities, the higher incidence of brucellosis among men in rural areas may be attributed to these factors. However, in urban areas, women are more likely to be infected due to their involvement in cooking and increased contact with livestock products. For brucellosis, the incidence during the first six months of the year, notably in May (47 cases out of 258 individuals), exceeded that in the latter six months, particularly in February (9 cases out of 258 individuals). This trend is attributed to the calving of livestock and the subsequent rise in milk and dairy production, such as yogurt, during this period. The consumption of unpasteurized milk and contaminated dairy products elevates the risk of infection. Moreover, the increased number of births heightens the probability of contact with livestock farmers or those handling the animals, serving as a direct risk factor (16). In a similar study conducted by Ghasemi et al. in Kurdistan province, the most common months for the occurrence of the disease in the first six months of the year were April (1.12%) and May (9.11%), while the lowest prevalence in the second six months, especially in November (0.84%) (12). Because of the young population, this group's work in the village, and their contact with livestock, the age group most affected is the 29-20 age group. In a similar study, Zeinali et al. found that the highest age group corresponds to the 30-20 years age range (17). In the present study, the highest frequency of titers for Wright, 2ME, and Combs is 1:160, 1:160, and 1:180, respectively. However, in a study conducted by Farahani et al., the highest frequency of titers for Wright and 2ME among patients is 1:320 and 1:80, respectively (15). The most common clinical symptom for most patients was musculoskeletal pain (95%), with weight loss being the least common symptom (5%). In a similar study conducted by Nabavi et al. in the Kohgiluyeh and Boyer-Ahmad provinces, prevalent clinical symptoms included musculoskeletal pain (74%), fever (58%), back pain (55%), weakness and loss of appetite (42%), weight loss (32%), depression (1.2%), and fatigue and malaise (7.5%) (18). The majority of patients (86%) were infected through the consumption of contaminated milk, and the highest incidence of infection is associated with rural areas. In a similar study conducted by Ghasemi et al. in Kurdistan province, the most common mode of transmission of the disease was the consumption of contaminated dairy products in conjunction with contact with livestock. This may be explained by the higher prevalence in rural areas. In urban areas, the consumption of contaminated dairy products is the most common mode of transmission (12).
Conclusion
The high prevalence of brucellosis in rural areas, particularly among rural men, suggests that this group lacks awareness of the modes of disease transmission. Improved education can raise awareness levels among rural residents about this disease. Strategies such as mechanizing livestock farming, providing ongoing education, and implementing more robust environmental health measures can help reduce the spread of the disease.
Acknowledgement
We would like to express our sincere gratitude to the staff at the Behbahan County Health Center for their support in data collection. We are grateful to the Behbahan Faculty of Medical Sciences for providing us with the necessary resources and financial support (Research code: 4032, The date of approval: 2022-05-30).
Funding sources
This work received financial support from the Vice-Chancellor of Research and Technology at Behbahan Faculty of Medical Sciences.
Ethical statement
This article was supported and approved by the Ethics Committee of the Behbahan Faculty of Medical Sciences (Ethics code: IR.BHN.REC.1401.011). Patients’ data were de-identified to protect the privacy and confidentiality of the participants.
Conflicts of interest
None.
Author contributions
Conceptualization: AJ and KAB. Data curation: MJ and AD. Formal Analysis: RG and MP. Funding acquisition: AJ. Investigation: MS and AJ. Methodology: MS, AJ, and KAB. Project administration and resources: AJ. Software: AJ, KAB, and ZN. Supervision: MS and AJ. Validation and visualization: MS and AJ. Writing original draft: ZN and AJ. Writing review and editing: RS and AJ.
Full-Text: (42 Views)
Introduction
Brucellosis is a zoonotic disease transmitted to humans through infected animals such as cattle, goats, and sheep, and by unpasteurized dairy products. The disease is caused by bacteria of the genus Brucella, including Brucella melitensis, Brucella abortus, and Brucella suis, which cause disease in humans. It can also be transmitted from animals to humans through direct contact, unpasteurized/raw dairy products, and airborne particles (1,2). Brucellosis in humans can cause localized purulent infection in the liver, spleen, bones, and some other organs. Because of its long-term complications, it is known as the disease of a thousand faces (3). Symptoms of the disease include persistent or recurrent fever with intermittent episodes, excessive night sweating, weight loss, headache, muscle aches, loss of appetite, and body aches (4). Brucellosis is a zoonosis affecting approximately 500,000 people worldwide annually, of which only 10-4% occur in developed countries, possibly due to the implementation of vaccination-based control programs. However, brucellosis remains a serious health problem in less developed countries. Recent reports indicate that brucellosis is endemic or potentially endemic in 179 countries worldwide. The disease remains a major health problem in the Mediterranean region, the Middle East, Western Asia, parts of Africa, and Latin America (5,6). The epidemiology of brucellosis is complex, and Latin American countries such as Mexico and Peru have reported a large number of cases; the same pattern applies to Mediterranean countries such as Iran, Russia, Mongolia, and Syria, which have the highest annual incidence of human brucellosis. Brucellosis is recognized as an endemic or indigenous disease in Iran; however, its incidence is not uniform across all provinces, with higher rates reported in certain regions. Provinces such as Zanjan, Hamedan, Markazi, and East Azerbaijan have reported the highest incidence of the disease, while southern provinces have reported lower rates (7,8). This study aimed to investigate the epidemiologic, demographic, and clinical characteristics of brucellosis in Behbahan County, southwestern Iran, during 2000-2021.
Methods
The present study was a retrospective population-based study conducted in Behbahan County. The study population consisted of 258 patients who were followed up and treated based on medical examination and history and with laboratory diagnosis of brucellosis, and who were identified by the private and public sectors from 2000 to 2021, and who had completed the brucellosis form. In the disease surveillance system in Iran, for all individuals to actively participate in disease reporting and also for the coordination and uniformity of measures at the national level, definitions have been developed for reportable diseases and their reporting methods. Based on symptoms and test results, diseases are classified (Suspected, probable, and definite), and these definitions are used throughout the country to report diseases to higher levels. Brucellosis is classified as a non-urgent reportable disease. It is reported monthly from environmental levels (Comprehensive health centers, health bases, health homes, government hospitals, and government laboratories) to the county health center. At the county health center, disease cases are registered on the Ministry of Health's Health Deputy's portal. A comprehensive questionnaire was developed to collect key factors such as age, sex, disease onset, occupation, history of contact with livestock, location of residence, consumption history of unpasteurized dairy products, intake of various dairy products, time of disease reporting, and results of Wright, Coombs, and 2ME tests. The study examined patient data reported through the health network of Behbahan University of Medical Sciences from 2000 to 2021. After collecting the data, they were entered into Excel software and then the variables were coded. SPSS software version 21 was used to analyze the data. To describe the variables, central and dispersion indices were used, and for nominal and ordinal variables, absolute and relative frequencies were used, and the Chi-square and T-test statistical tests were used to analyze the data.
Results
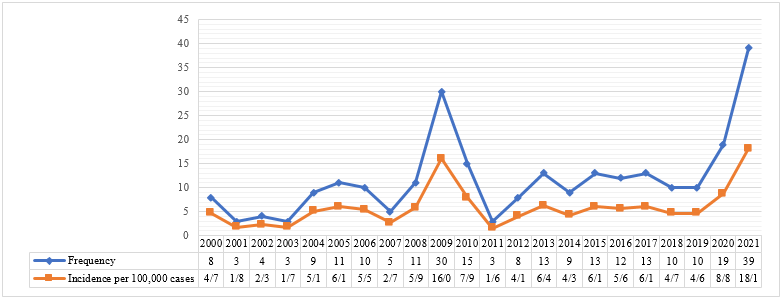
The results showed that the highest and the lowest number of cases per 100,000 population were reported in 2021 (39 cases, 1.18%) and 2010 (3 cases, 0.61%), respectively. The average incidence rate (Per 100,000 population) was six (Figure 1). The highest clinical manifestations of the disease occurred between May (47 cases) and June (36 cases), while the lowest occurrences were observed between February (9 cases) through December (10 cases). The findings showed that 137 (Out of 258) cases (53%) of the patients were men. In terms of residence distribution, there were 139 rural individuals (54%) and 119 urban individuals (46%). As observed, the overall incidence of disease is higher in the rural population than in the urban population. In treating brucellosis, Rifampin and Doxycycline are the most commonly used drugs (100%), while Gentamicin has the lowest use rate (3.2%). For the 2ME test, most patients had a titer of 1/160. For the Coombs test, most patients had a titer of 1/80; for the Wright test, most patients had a titer of 1/160. The most observed clinical symptom in patients was bone and muscle pain (n=245, 95%). More details about the clinical symptoms of the patients are illustrated in Figure 2. In the present study, 58 cases (20%) had a history of hospitalization. The longest duration of hospitalization (17 days) was observed in one case, while the shortest (1 day) was reported in five cases. When potential risk factors were examined, 171 cases (66%) had a history of contact with livestock or their products. The history of using unsterilized animal products was reported in 229 cases (88.8%), contact with live animals in 156 cases (60.5%), animal slaughter and contact with blood and secretions in 34 cases (13.2%), and keeping livestock at home in 107 cases (41.4%). Based on the study's results, the highest prevalence of the disease was observed in livestock farmers (n=108, 41.9%). More details are summarized in Table 1. Most patients, 224 cases (86.86%), attribute their illness to milk consumption. Moreover, rural areas show the highest case count. In terms of age, there were 11 cases in the 0-9 years range, 32 cases in the 10-19 years range, 48 cases in the 20-29 years range, 47 cases in the 30-39 years range, 44 cases in the 40-49 years range, 36 cases in the 50-59 years range, 29 cases in the 60-69 years range, and 11 cases in the 70 years and above range. The highest prevalence was observed in the 20-29 age group.
Brucellosis is a zoonotic disease transmitted to humans through infected animals such as cattle, goats, and sheep, and by unpasteurized dairy products. The disease is caused by bacteria of the genus Brucella, including Brucella melitensis, Brucella abortus, and Brucella suis, which cause disease in humans. It can also be transmitted from animals to humans through direct contact, unpasteurized/raw dairy products, and airborne particles (1,2). Brucellosis in humans can cause localized purulent infection in the liver, spleen, bones, and some other organs. Because of its long-term complications, it is known as the disease of a thousand faces (3). Symptoms of the disease include persistent or recurrent fever with intermittent episodes, excessive night sweating, weight loss, headache, muscle aches, loss of appetite, and body aches (4). Brucellosis is a zoonosis affecting approximately 500,000 people worldwide annually, of which only 10-4% occur in developed countries, possibly due to the implementation of vaccination-based control programs. However, brucellosis remains a serious health problem in less developed countries. Recent reports indicate that brucellosis is endemic or potentially endemic in 179 countries worldwide. The disease remains a major health problem in the Mediterranean region, the Middle East, Western Asia, parts of Africa, and Latin America (5,6). The epidemiology of brucellosis is complex, and Latin American countries such as Mexico and Peru have reported a large number of cases; the same pattern applies to Mediterranean countries such as Iran, Russia, Mongolia, and Syria, which have the highest annual incidence of human brucellosis. Brucellosis is recognized as an endemic or indigenous disease in Iran; however, its incidence is not uniform across all provinces, with higher rates reported in certain regions. Provinces such as Zanjan, Hamedan, Markazi, and East Azerbaijan have reported the highest incidence of the disease, while southern provinces have reported lower rates (7,8). This study aimed to investigate the epidemiologic, demographic, and clinical characteristics of brucellosis in Behbahan County, southwestern Iran, during 2000-2021.
Methods
The present study was a retrospective population-based study conducted in Behbahan County. The study population consisted of 258 patients who were followed up and treated based on medical examination and history and with laboratory diagnosis of brucellosis, and who were identified by the private and public sectors from 2000 to 2021, and who had completed the brucellosis form. In the disease surveillance system in Iran, for all individuals to actively participate in disease reporting and also for the coordination and uniformity of measures at the national level, definitions have been developed for reportable diseases and their reporting methods. Based on symptoms and test results, diseases are classified (Suspected, probable, and definite), and these definitions are used throughout the country to report diseases to higher levels. Brucellosis is classified as a non-urgent reportable disease. It is reported monthly from environmental levels (Comprehensive health centers, health bases, health homes, government hospitals, and government laboratories) to the county health center. At the county health center, disease cases are registered on the Ministry of Health's Health Deputy's portal. A comprehensive questionnaire was developed to collect key factors such as age, sex, disease onset, occupation, history of contact with livestock, location of residence, consumption history of unpasteurized dairy products, intake of various dairy products, time of disease reporting, and results of Wright, Coombs, and 2ME tests. The study examined patient data reported through the health network of Behbahan University of Medical Sciences from 2000 to 2021. After collecting the data, they were entered into Excel software and then the variables were coded. SPSS software version 21 was used to analyze the data. To describe the variables, central and dispersion indices were used, and for nominal and ordinal variables, absolute and relative frequencies were used, and the Chi-square and T-test statistical tests were used to analyze the data.
Results
The results showed that the highest and the lowest number of cases per 100,000 population were reported in 2021 (39 cases, 1.18%) and 2010 (3 cases, 0.61%), respectively. The average incidence rate (Per 100,000 population) was six (Figure 1). The highest clinical manifestations of the disease occurred between May (47 cases) and June (36 cases), while the lowest occurrences were observed between February (9 cases) through December (10 cases). The findings showed that 137 (Out of 258) cases (53%) of the patients were men. In terms of residence distribution, there were 139 rural individuals (54%) and 119 urban individuals (46%). As observed, the overall incidence of disease is higher in the rural population than in the urban population. In treating brucellosis, Rifampin and Doxycycline are the most commonly used drugs (100%), while Gentamicin has the lowest use rate (3.2%). For the 2ME test, most patients had a titer of 1/160. For the Coombs test, most patients had a titer of 1/80; for the Wright test, most patients had a titer of 1/160. The most observed clinical symptom in patients was bone and muscle pain (n=245, 95%). More details about the clinical symptoms of the patients are illustrated in Figure 2. In the present study, 58 cases (20%) had a history of hospitalization. The longest duration of hospitalization (17 days) was observed in one case, while the shortest (1 day) was reported in five cases. When potential risk factors were examined, 171 cases (66%) had a history of contact with livestock or their products. The history of using unsterilized animal products was reported in 229 cases (88.8%), contact with live animals in 156 cases (60.5%), animal slaughter and contact with blood and secretions in 34 cases (13.2%), and keeping livestock at home in 107 cases (41.4%). Based on the study's results, the highest prevalence of the disease was observed in livestock farmers (n=108, 41.9%). More details are summarized in Table 1. Most patients, 224 cases (86.86%), attribute their illness to milk consumption. Moreover, rural areas show the highest case count. In terms of age, there were 11 cases in the 0-9 years range, 32 cases in the 10-19 years range, 48 cases in the 20-29 years range, 47 cases in the 30-39 years range, 44 cases in the 40-49 years range, 36 cases in the 50-59 years range, 29 cases in the 60-69 years range, and 11 cases in the 70 years and above range. The highest prevalence was observed in the 20-29 age group.
Discussion
Although brucellosis has been eradicated in some countries, it still exists as an endemic health problem in our country (9). According to the WHO, the incidence of this disease ranges from 0.01 to 200 per 100,000 people, and the prevalence varies from 0.5 per 100 people to 9.10 per 100 people in different provinces of Iran (10). Based on the findings of this study, the incidence of brucellosis in Behbahan County during the period of 2000-2021 was an average of 0.6 per 100,000 individuals. A similar study conducted by Jelastopulu et al. demonstrated that through vaccination of livestock and public education in western Greece the incidence of brucellosis could be reduced from 10 per 100,000 individuals (1998-1997) to 0.3 per 1,000 individuals (2002-2000) (11). The history of patient contact with livestock and unsterilized livestock products, especially unsterilized dairy products, had the highest percentage (88.8%), while the lowest percentage (13.02%) was related to contact with animal slaughter, blood, and secretions. This may indicate that the climatic characteristics of Behbahan County contribute to a higher presence of livestock in the region, which in turn leads to more opportunities for contact with livestock. In a similar study conducted by Ghasemi et al. in Kurdistan province, the most common mode of disease transmission was contact with contaminated animals and the consumption of contaminated animal products (48.3%). Disease transmission by eating contaminated animal products alone (7.36%) or by contact with contaminated animals alone (6.10%) had a lower prevalence (12). Livestock farmers account for 42% of the patients compared to other occupations in Behbahan County, confirming the previous conclusion that the level of contact with livestock is high in the region. In a similar study conducted by Shahriari et al. in Kohgiluyeh and Boyer-Ahmad provinces in 2009-2013, it was found that 84% had a history of contact with livestock, and 31.5% were livestock farmers or slaughterhouse workers (6). In this study, men (53%) were more affected than women (47%). A study conducted by Hosseini et al. in Amol County also showed a higher incidence in males compared to females (13). Another study conducted by Hamzavi et al. in Kermanshah province showed a higher incidence in males compared to females, which is consistent with the current study (14). The higher incidence of brucellosis in men compared to women is probably attributed to the type of work and increased contact with livestock and their products. In the current study, the majority of cases were rural residents (54%). In a similar study conducted by Hosseini et al. in Amol County, the incidence of brucellosis was higher among rural residents (68.21%) compared to urban residents (31.79%) (13). In another similar study conducted by Farahani et al. in Arak County, the majority of brucellosis cases were among rural residents (72%) compared to urban residents (28%) (15). The overall incidence of brucellosis was higher in the rural population compared to the urban population. There is a significant association between gender and livestock. In rural populations, the incidence of brucellosis is higher in men than women, and contact with livestock is likely considered a primary mode of transmission for women in these areas. Since contact with livestock and handling of fetal products is more likely to be performed by men in the current living conditions of rural communities, the higher incidence of brucellosis among men in rural areas may be attributed to these factors. However, in urban areas, women are more likely to be infected due to their involvement in cooking and increased contact with livestock products. For brucellosis, the incidence during the first six months of the year, notably in May (47 cases out of 258 individuals), exceeded that in the latter six months, particularly in February (9 cases out of 258 individuals). This trend is attributed to the calving of livestock and the subsequent rise in milk and dairy production, such as yogurt, during this period. The consumption of unpasteurized milk and contaminated dairy products elevates the risk of infection. Moreover, the increased number of births heightens the probability of contact with livestock farmers or those handling the animals, serving as a direct risk factor (16). In a similar study conducted by Ghasemi et al. in Kurdistan province, the most common months for the occurrence of the disease in the first six months of the year were April (1.12%) and May (9.11%), while the lowest prevalence in the second six months, especially in November (0.84%) (12). Because of the young population, this group's work in the village, and their contact with livestock, the age group most affected is the 29-20 age group. In a similar study, Zeinali et al. found that the highest age group corresponds to the 30-20 years age range (17). In the present study, the highest frequency of titers for Wright, 2ME, and Combs is 1:160, 1:160, and 1:180, respectively. However, in a study conducted by Farahani et al., the highest frequency of titers for Wright and 2ME among patients is 1:320 and 1:80, respectively (15). The most common clinical symptom for most patients was musculoskeletal pain (95%), with weight loss being the least common symptom (5%). In a similar study conducted by Nabavi et al. in the Kohgiluyeh and Boyer-Ahmad provinces, prevalent clinical symptoms included musculoskeletal pain (74%), fever (58%), back pain (55%), weakness and loss of appetite (42%), weight loss (32%), depression (1.2%), and fatigue and malaise (7.5%) (18). The majority of patients (86%) were infected through the consumption of contaminated milk, and the highest incidence of infection is associated with rural areas. In a similar study conducted by Ghasemi et al. in Kurdistan province, the most common mode of transmission of the disease was the consumption of contaminated dairy products in conjunction with contact with livestock. This may be explained by the higher prevalence in rural areas. In urban areas, the consumption of contaminated dairy products is the most common mode of transmission (12).
Conclusion
The high prevalence of brucellosis in rural areas, particularly among rural men, suggests that this group lacks awareness of the modes of disease transmission. Improved education can raise awareness levels among rural residents about this disease. Strategies such as mechanizing livestock farming, providing ongoing education, and implementing more robust environmental health measures can help reduce the spread of the disease.
Acknowledgement
We would like to express our sincere gratitude to the staff at the Behbahan County Health Center for their support in data collection. We are grateful to the Behbahan Faculty of Medical Sciences for providing us with the necessary resources and financial support (Research code: 4032, The date of approval: 2022-05-30).
Funding sources
This work received financial support from the Vice-Chancellor of Research and Technology at Behbahan Faculty of Medical Sciences.
Ethical statement
This article was supported and approved by the Ethics Committee of the Behbahan Faculty of Medical Sciences (Ethics code: IR.BHN.REC.1401.011). Patients’ data were de-identified to protect the privacy and confidentiality of the participants.
Conflicts of interest
None.
Author contributions
Conceptualization: AJ and KAB. Data curation: MJ and AD. Formal Analysis: RG and MP. Funding acquisition: AJ. Investigation: MS and AJ. Methodology: MS, AJ, and KAB. Project administration and resources: AJ. Software: AJ, KAB, and ZN. Supervision: MS and AJ. Validation and visualization: MS and AJ. Writing original draft: ZN and AJ. Writing review and editing: RS and AJ.
Type of Article: Brief Report |
Subject:
Epidemiology
Received: 2024/09/3 | Accepted: 2024/12/12 | Published: 2024/12/31
Received: 2024/09/3 | Accepted: 2024/12/12 | Published: 2024/12/31
References
1. Qie C, Cui J, Liu Y, Li Y, Wu H, Mi Y. Epidemiological and clinical characteristics of bacteremic brucellosis. J Int Med Res. 2020;48(7):300060520936829. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Varikkodan I, Naushad VA, Purayil NK, Zahid M, Sirajudeen J, Ambra N, et al. Demographic characteristics, laboratory features and complications in 346 cases of brucellosis: A retrospective study from Qatar. IJID Reg. 2023;10:18-23. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Liang C, Wei W. [Analysis of clinical characteristics of 129 acute and chronic occupational brucellosis in HulunBuir City]. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2024;42(3):195-198. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Li D, Yuan G, Wang YO, Wang H, Zhang Q, Wang YA, et al. Clinical Characteristics, Treatment, and Prognosis of Osteoarticular Brucellosis: A Retrospective Real-World Study in Shenyang, China, 2014-2019. Foodborne Pathog Dis. 2024. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Elbehiry A, Aldubaib M, Marzouk E, Abalkhail A, Almuzaini AM, Rawway M, et al. The Development of Diagnostic and Vaccine Strategies for Early Detection and Control of Human Brucellosis, Particularly in Endemic Areas. Vaccines. 2023;11(3):654. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Shahriari S, Ghatee M, Haghdoost A, Taabody Z, Khajeh Kazemi R, Parisae Z, et al. Demographic and epidemiological study of brucellosis in the Kohgiluyeh and Boyer-Ahmad province, 2009-2013. Armaghane Danesh. 2015;20(2):149-60. [View at Publisher] [Google Scholar]
7. Bagheri H, Tapak L, Karami M, Amiri B, Cherghi Z. Epidemiological features of human brucellosis in Iran (2011-2018) and prediction of brucellosis with data-mining models. J Res Health Sci. 2019;19(4):e00462. [View at Publisher] [PMID] [Google Scholar]
8. Jokar M, Rahmanian V, Golestani N, Raziee Y, Farhoodi M. The global seroprevalence of equine brucellosis: a systematic review and meta-analysis based on publications from 1990 to 2022. J Equine Vet Sci. 2023;123:104227. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Kaboli Boroujeni H, Abutalebi MS, Kheirollahi N, Haghighat S. Epidemiological surveillance of livestock brucellosis in Borujen County during 2010 - 2016. Iran J Vet Med. 2020;14(1):41-50. [View at Publisher] [Google Scholar]
10. Narimisa N, Razavi S, Masjedian Jazi F. Risk Factors Associated with Human Brucellosis: A Systematic Review and Meta-Analysis. Vector Borne Zoonotic Dis. 2024;24(7):403-410 [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Jelastopulu E, Bikas C, Petropoulos C, Leotsinidis M. Incidence of human brucellosis in a rural area in Western Greece after the implementation of a vaccination programme against animal brucellosis. BMC Public Health. 2008;8:241. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Ghasemi B, Mohammadia B, Soofimajidpour M. Epidemiology of Human and Animal Brucellosis in Kurdistan Province in 1997-2001. Sci J Kurdistan Univ Med. 2003;8(2):24-32. [Persian] [View at Publisher] [Google Scholar]
13. Hosseini SM, Amani R, Razavimehr SV, Moshrefi A, Aghajanikhah MH, Mahmoodi P. Epidemiology of Brucellosis in Amol City from 2011 to 2013. Beyhagh. 2016;21(1):1-7. [Persian] [View at Publisher] [Google Scholar]
14. Hamzavi Y, Khademi N, Ghazi Zadeh MM, Janbakhsh A. Epidemiology of malt fever in Kermanshah province in 2011. J Kermanshah Uni Med Sci. 2014;18(2):114-21. [View at Publisher] [Google Scholar]
15. Farahani S, Shah Mohamadi S, Navidi I, Sofian M. An investigation of the epidemiology of brucellosis in Arak City, Iran, (2001-2010). J Arak Uni Med Sci. 2012;14(7):49-54. [View at Publisher] [Google Scholar]
16. Bagbanian M, Momayyezi M, Fallahzadeh H, Mirzaei M. Prevalence of illicit drug use and related factors in adults: results of the first phase of Shahedieh Cohort Study 2015-2016. Iran J Epidemiol. 2022;17(4):353-61. [View at Publisher] [DOI] [Google Scholar]
17. Zeinali M, Shirzadi MR. Effective ingredient in accretion and reduction of brucellosis incidence in humans in Iran in 1985-2005. 15th Veterinary Congress. 2008. [Persian] [View at Publisher] [Google Scholar]
18. Nabavi M, Hatami H, Jamali Arand HA. Epidemiological, Clinical and Paraclinical Surveys of Children and Adolescents with Brucellosis in Kohgiluyeh and Boyer Ahmad Province in Southwest of Iran during 2009-2015. Armaghane Danesh. 2018;10;23(2):236-52. [View at Publisher] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |